RELEASE THE PAIN, BE MORE ALIVE

Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor
incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam

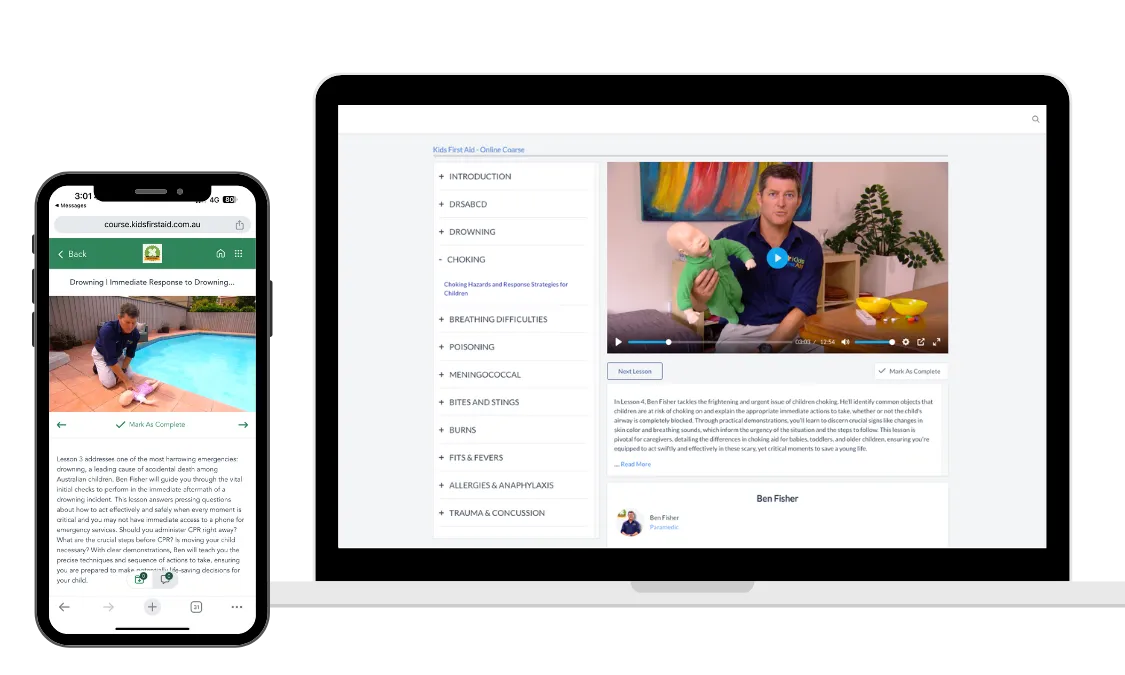
Learn Life-Saving First Aid for Kids
from Experienced Paramedics
The Startling Reality
Children's Safety at Stake
Children are surprisingly vulnerable to accidents within the safety of their homes. Injuries are the leading cause of death in Australian children, with one in 13 children visiting hospitals for injuries each year. More children succumb to injuries than to cancer, asthma, and infectious diseases combined. Our course addresses this alarming situation by empowering you with the knowledge and skills to prevent and respond to these common yet preventable accidents.



Your misalignment needs our adjustment.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.

Consultations
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor

Choose Date
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor

Meet the Doctor
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor

Treatments
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor

Expert Training for Everyday Heroes
Our course offers practical, paramedic-led training, covering the most common emergencies such as choking, breathing difficulties, burns, and scalds. With over 150,000 Australian children visiting hospital emergency rooms annually for accidents like falls, poisoning, and burns, this training is not just a course – it's essential preparation for all parents.

Trusted Knowledge from Frontline Experts
Join Ben Fisher, a seasoned paramedic and the co-founder of Kids First Aid, in this vital introduction to child-focused first aid. This lesson is specifically crafted for parents, grandparents, and caregivers, aiming to equip them with the crucial skills needed to tackle the most common emergency scenarios children encounter. From treating burns to managing insect bites and effectively administering CPR, this course empowers you with the knowledge to respond to urgent situations with assurance and calm. Discover life-saving techniques that can make a profound difference in moments of crisis and gain the confidence to provide care when it matters most.
Comprehensive First Aid Coverage for Every Parent

Introduction
Meet Ben Fisher, a paramedic and father, who will guide you through identifying and responding to common dangers.

Emergency Response Protocol
Learn the vital steps of DRSABCD to act swiftly and effectively in emergencies.

Water Safety & Rescue
Gain critical skills to prevent and respond to drowning incidents.

Choking Hazards & Intervention
Understand how to react when a child is choking to save lives in seconds.

Managing Respiratory Emergencies
Learn the vital steps of DRSABCD to act swiftly and effectively in emergencies.

Poison Control & Care
Learn how to deal with poisoning to minimise risk and maximise safety.

Tackling Meningococcal Disease
Identify and respond to meningococcal disease swiftly to protect your child.

Insect Bites and Animal Stings
Effective treatments for bites and stings that every parent should know.

Burns: Prevention and Treatment
Comprehensive strategies for dealing with burns and promoting healing.

Seizures and High Fevers
Recognise and manage febrile seizures and high fevers with expert guidance.

Allergy & Anaphylaxis Management
Be prepared for allergic reactions with life-saving interventions.

Addressing Trauma & Head Injuries
Crucial techniques for managing trauma and concussions in children.
Lifetime Access
Only $89
Adjust Your Body Get A Perfect Balance

Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat Duis aute irure dolor
Learn from customer feedback
24/7 customer support
Professional Team
High Savings Potenstial
Book Your
Appointment
The sky was cloudless and of a deep dark blue spectacle before us was indeed sublime.
Our Services
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod
tempor incididunt ut labore et dolore magna aliqua.

Back Adjustment
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore

Muscle Injury
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore

Body Massage
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore

Bone Injury
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore

Acupunture
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore

Body Adjustment
Lorem ipsum dolor sit amet, consect adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore
Guarantee Feel Free From Pain Again
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.

Affordable Price
Lorem ipsum dolor sit amet, consectetur
adipiscing elit, sed do eiusmod tempor incididunt ut labore et

Best Service
Lorem ipsum dolor sit amet, consectetur
adipiscing elit, sed do eiusmod tempor incididunt ut labore et

Humble Therapist
Lorem ipsum dolor sit amet, consectetur
adipiscing elit, sed do eiusmod tempor incididunt ut labore et
What students say about us

About an hour ago my 2 year old daughter swallowed a 5 cent
piece and wasn't able to breathe. The look on her face was terrifying. Thankfully, you helped me be prepared and know what to do. After the 5 back blows she spluttered, wretched and must've gotten the coin out of her airway as she started breathing again. It was honestly the most terrifying thing I've been through with my kids.
Thanks again for giving me the information to be able to handle the situation.
Nancie

I was amazed at how logical and simple so many first aid steps
for various situations are! Things have changed since learning all those complicated and confusing procedures in P.E. at high school! After realising how simple (and obviously life-changing) first aid really is I cannot help but wonder why it isn't compulsory for everyone to learn first aid! The fee is peanuts when compared to the value of what is learnt.
Mandy Clarke

Frequently Asked Question
What do you cover in your courses?
Our courses cover the 10 most common household emergency situations our paramedics see that involve children. eg. Choking, burns, drowning, factures, bleeding, and poisoning. All the things parents worry about!
Are your courses accredited?
We have found most parents don’t have the full day required to complete an accredited first aid course, let alone the pre work and subsequent evaluation. That’s why we developed a concise 3 hour workshop covering all the essential skills parents require to avoid a tragedy in the home. Our courses are delivered exclusively by paramedics able to transfer their firsthand knowledge and expertise. While we take our content very seriously, we also ensure it is delivered in a practical and engaging manner in a relaxed environment. Accredited courses are available by request. Please call 1300 138 133 for more information.
Is there an exam? Do I need to take notes?
No, there is no exam in our 3 hr session and no need to take notes. The course is designed to give you simple, practical and current skills that you can use in an emergency. For this reason we don't teach the course in a way you need to 'study'.
To what child age group is your course applicable?
Our courses are aimed at parents/carers of children 0-16 yrs. However, the first aid techniques we cover are relevant to all ages. Even adults!
What's the difference between your courses and other first aid courses?
All our sessions are presented by trained and experienced paramedics - who are absolute experts in emergency care! They have experience treating parents and children on an ongoing basis, for all the situations we cover, including choking, drowning, burns, fits, fractures, bleeding, fits and poisonings.
Do you cover CPR?
Yes. The first section of the course covers CPR. We also demonstrate the difference between implementing CPR on a new born baby vs a toddler vs a child vs an adult. You will not be individually assessed.
What client say about us

Lorem Ipsum is simply dummy text of the printing and typesetting industry. Lorem Ipsum has been the industry's standard dummy text ever since the 1500s, when an unknown printer took a galley of type and scrambled.

Darcel Ballentine
Barone LLC.

Lorem Ipsum is simply dummy text of the printing and typesetting industry. Lorem Ipsum has been the industry's standard dummy text ever since the 1500s, when an unknown printer took a galley of type and scrambled.

Leatrice Handler
Acme Co.
BOOK YOUR APPOINTMENT
The sky was cloudless and of a deep dark blue spectacle before us was indeed sublime.



